Clinical Trials in mCNV
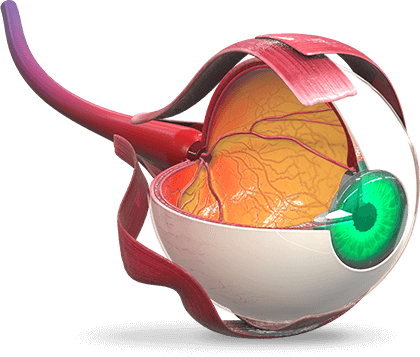
Overview of Disease State
Simple myopia is frequently corrected via contact lenses, spectacles, or refractive surgery. Some patients with high myopia, however, will develop progressive high myopia, a disorder defined by continual and progressive retinal degeneration. A significant complication of both high myopic and pathologic high myopia is myopic choroidal neovascularization (mCNV), which results in acute deterioration of central visual acuity (VA) due to the development of subretinal/choroidal neovascularization (CNV). [Willis.Ophthalmology.2016]
Visual prognosis is poor. [Ikuno.Ophthalmology.2015] Myopic CNV affects people of Asian descent disproportionately to other ethnicities. In patients with pathologic myopia, the risk of developing mCNV is 5% to 11%, and for those with preexisting mCNV, about 30% will develop CNV in the fellow eye within a span of 8 years. [Chen.Retina.2019] Of particular concern, mCNV is a frequent cause of vision impairment in patients aged less than 50 years. Close to 90% of patients will have a VA of 20/200 or less after 5 years following diagnosis. [Ikuno.Ophthalmology.2015]
Ranibizumab was the first anti-vascular endothelial growth factor (VEGF) agent to be approved for the treatment of visual impairment due to CNV secondary to pathologic myopia (in 2013 in the European Union and in 2017 in the United States), based on the results from the 12-month, phase 3 RADIANCE study.[Chen.Retina.2019] International studies analyzing the impact of additional anti-VEGF agents (aflibercept, conbercept, and pegaptanib), as well as the effect of alternative approaches including verteporfin photodynamic therapy (vPDT) and vitrectomy, on the clinical course of mCNV in various populations have previously or are currently under investigation.
Click on the study name to see more details about each particular study. To enhance visibility of graphs and tables, click on the image to enlarge for expanding viewing.
Myopic Choroidal Neovascularization Clinical Studies (anti-VEGF and PDT)
References
Chen Y, Sharma T, Li X, et al. Ranibizumab versus verteporfin photodynamic therapy in Asian patients with myopic choroidal neovascularization: Brilliance, a 12-month, randomized, double-masked study. Retina. 2018;39(10):1885-1994. https://doi.org/10.1097/IAE.0000000000002292
Erden B, Bolukbasi S, Bas E, Cakir A. Comparison of intravitreal aflibercept and ranibizumab for treatment of myopic choroidal neovascularization: one-year results — a retrospective, comparative study. J Ophthalmol. 2019;2019:8639243. doi:10.1155/2019/8639243
Ikuno Y, Ohno-Matsui K, Wong TY, et al. Intravitreal aflibercept injection in patients with myopic choroidal neovascularization: the MYRROR study. Ophthalmology. 2015;122(6):1220-1227.
Jain M, Narayanan PJ, Mohamed A, et al. Incidence, predictors and re-treatment outcomes of recurrent myopic choroidal neo-vascularization. PLOS One. 2022;17:e0271342. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0271342
Tufail A, Narendran N, Patel PJ, et al. Ranibizumab in myopic choroidal neovascularization: the 12-month results from the REPAIR study. Ophthalmology. 2013;120:1944-1945.
Verteporfin in Photodynamic Therapy Study Group. Photodynamic therapy of subfoveal choroidal neovascularization in pathologic myopia with verteporfin. 1-year results of a randomized clinical trial—VIP report no. 1. Ophthalmology. 2001;108(5):841-852.
Willis JR, et al. The prevalence of myopic choroidal neovascularization in the United States: analysis of the IRIS(®) Data Registry and NHANES. Ophthalmology. 2016;123(8):1771-1782.
Wolf S, Balciuniene VJ, Laganovska G, et al. RADIANCE: randomized controlled study of ranibizumab in patients with choroidal neovascularization secondary to pathologic myopia. Ophthalmology. 2014;121:682-692.
Yoshida T, Ohno-Matsui K, Yasuzumi K, et al. Myopic choroidal neovascularization: a 10-year follow-up. Ophthalmology. 2003;110(7):1297-1305.